Accurate RAF Scores Through Real-Time RPM Data

Risk Adjustment Factor (RAF) scores are central to how health plans manage care and forecast costs. Yet, the path to accurate scoring remains challenging. Traditional retrospective reviews are costly and often leave gaps. Prospective chart chases improve accuracy but are still time-bound and miss the nuance of a member’s day-to-day health. That’s where Remote Patient Monitoring (RPM) is changing the game.
For health plans that own or partner closely with provider networks, RPM delivers a powerful opportunity to capture accurate, real-time clinical data. It’s no longer about looking back or hoping for documentation during a single visit. With RPM, you gain a continuous view into your members’ health, tracking chronic conditions like hypertension, diabetes, or heart failure with the frequency and context that traditional models lack.
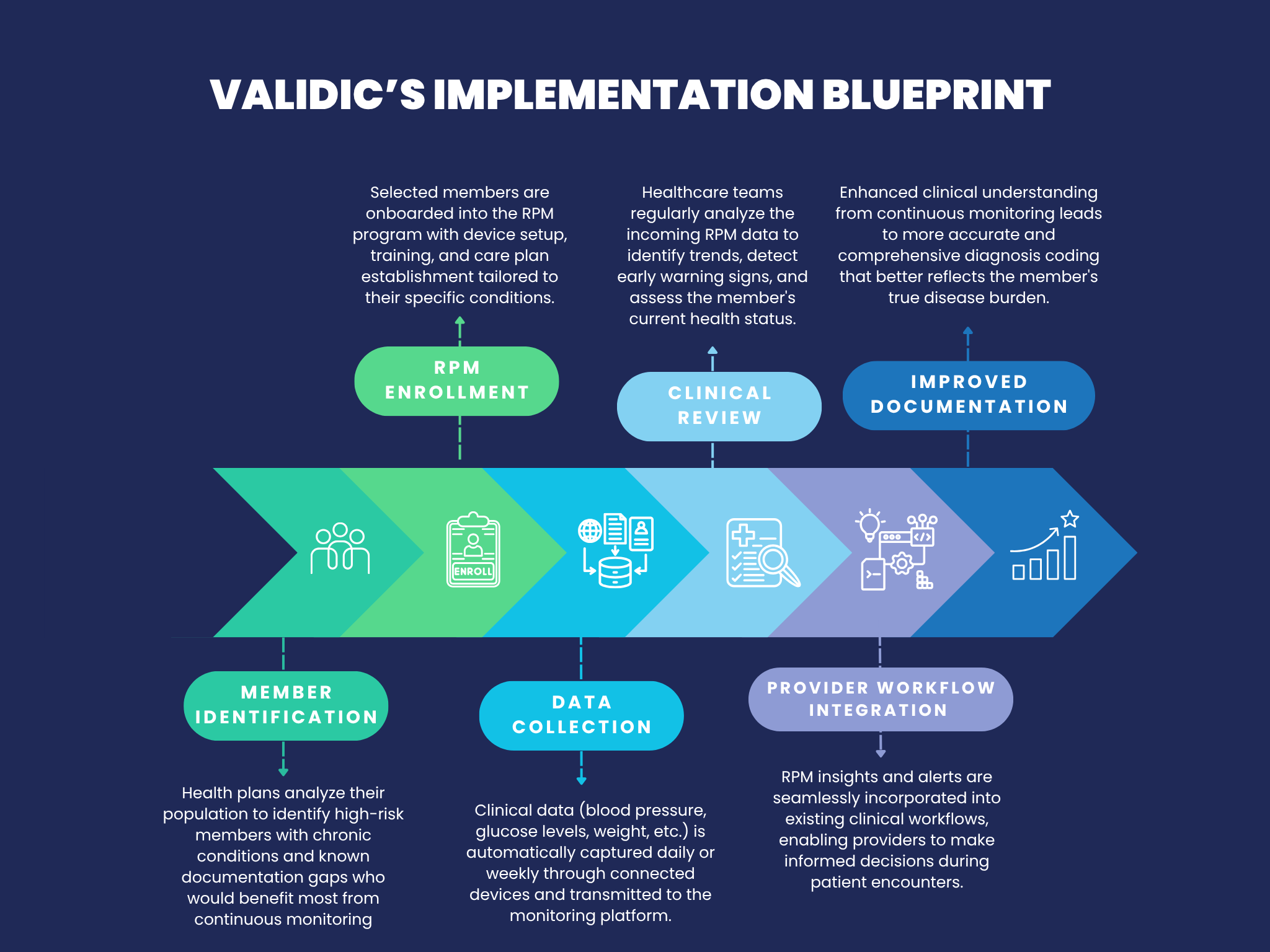
An effective blueprint for integrating RPM into a risk adjustment strategy starts with identifying high-value members—those with chronic conditions and known gaps in documentation. These members can be enrolled in RPM programs that collect biometric data daily or weekly. That data is then reviewed by clinical teams or surfaced in provider workflows, enabling timely outreach and more complete diagnosis capture. Over time, this model supports proactive coding, strengthens provider engagement, and ensures that documentation reflects true disease burden. The result is a more accurate RAF profile and fewer missed opportunities throughout the year.
CMS Endorsement of RPM
The Centers for Medicare & Medicaid Services (CMS) has increasingly supported RPM as a key tool in modern care delivery. It recognizes RPM as a reimbursable service for chronic condition management, signaling its clinical and operational value. By incorporating RPM into care models, organizations align with CMS’s emphasis on proactive, patient-centered care—one that prioritizes prevention, continuous monitoring, and timely intervention. This validation not only supports the use of RPM for improving outcomes but strengthens its role in accurate risk capture across populations.
Improving Care and Reducing Utilization
Beyond improving documentation, RPM is clinically impactful. It helps close care gaps for high-risk members, reinforces medication adherence, and enables timely interventions—avoiding costly events like emergency department visits or hospitalizations. For members, it leads to better outcomes. For health plans, it reduces unnecessary utilization while supporting quality performance.
Validic supports some of the most recognizable health plans in the country with RPM solutions that integrate seamlessly with provider workflows. To learn how your organization can leverage real-time RPM data to improve accuracy, close gaps, and reduce costs, reach out to us today.